A health care labyrinth: perspectives of caregivers on the journey to accessing timely cancer diagnosis and treatment for children in India | BMC Public Health

There were two critical phases in the family’s journey from symptom onset to the start of treatment: referral pathways taken to get to the treating hospital, and care after reaching the hospital. Table 2 shows three inter-related themes and their sub-themes which emerged from the data analysis. Thirty-nine caregivers were interviewed (15 in Hyderabad and 19 in New Delhi, with 6 interviews done in pairs) consisting of 17 fathers, 13 mothers, 7 uncles, 1 sister and 1 cousin. Interview duration in Hyderabad generally ranged from 9 to 20 min and 15 to 63 min in Delhi. Barriers identified in both cities did not largely differ and hence results are presented collectively across participants. Twenty-one caregivers were of lower SES and BPL and 13 from middle-upper SES. Patient sample consisted of 16 females and 18 males, aged between 6 months to 16 years. They were diagnosed with the following cancers: Acute Lymphoblastic Leukaemia (ALL), Acute Myeloid Leukaemia (AML), Non-Hodgkin Lymphoma, Brainstem glioma, Medulloblastoma, Neuroblastoma, Retinoblastoma, Wilms tumour, Rhabdomyosarcoma and Primitive Neuroectodermal Tumour (PNET). Distance to the treating hospital for families residing outside Delhi or Hyderabad was between 15 km – 1800 km, although total distance travelled could be greater due to varied referral pathways. More detail of demographics can be found in Additional file 1: Table S2.
Time: stop, slow down or speed up
The three sub-themes defined in this section were all crucial components which impacted upon the time taken to diagnose and treat the child. Sub-theme 1.1 refers to the multiple efforts and avenues undertaken by caregivers in visiting health care providers in the referral pathway before reaching the participating treating hospital. These efforts were influenced by determinants (1.2) such as suggestions by third parties or past experiences within the health system, and paucity of caregiver and health professional knowledge and awareness of childhood cancer. Upon reaching the treating hospital, families then spent time navigating their way through the hospital (1.3), which was also a contributor to time taken to receiving definitive diagnosis and care.
Efforts and avenues taken in the referral pathway
Families took multiple efforts and avenues to navigate the referral pathways. As shown in Fig. 1, those residing outside Delhi/Hyderabad had more complex pathways compared to those living within the city (Fig. 2). However, a few participants, residing within the city also experienced more erratic referral pathways consisting of complex visits. The first time interval occurred during the symptom onset stage. More prominent symptoms such as nose bleeds or blood in the urine prompted the family to seek immediate medical care, while some children with symptoms of fevers, runny nose or cough were treated at home with general medicines, postponing a visit to the doctor. Misdiagnoses such as: dengue, jaundice, rheumatoid arthritis, depression, typhoid, flu, chicken pox, pneumonia, diarrhoea and ulcers, also contributed to delay in reaching the cancer diagnosis. Recurring symptoms then triggered families to seek care with additional health care providers, including traditional healers and rural medical practitioners (RMP).
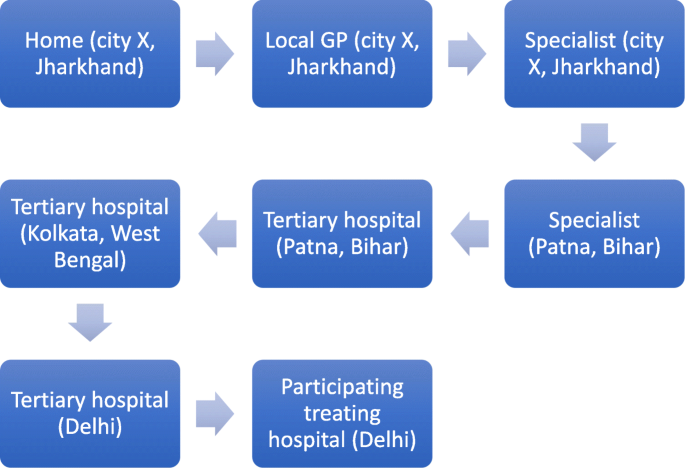
Typical referral pathway for most families traveling from other cities. This journey is an example of a child diagnosed with ALL in Delhi, belonging to a village in the state of Jharkhand who then travelled to cities within the states of West Bengal and Bihar before arriving in Delhi. Note: some of these pathways consisted of repeated visits

Typical referral pathway for most families residing within the same city as the participating treating centre. This journey is an example of a child diagnosed with AML in Hyderabad and a child diagnosed with Non-Hodgkin Lymphoma in Delhi. Note: some of these pathways consisted of repeated visits
Even though a few of the regional tertiary hospitals in north and south India were supposed to be able to treat children with cancer, in reality some basic services required were unavailable hence families were referred on. Caregivers often did not question the referrals, however some participants reported that health care providers explained the reason as being a lack of essential diagnostic facilities. Sometimes, caregivers themselves sought other avenues of care due to long admission waiting times or lack of money. One caregiver (Fig. 1) from the state of Jharkhand (approx. 1200 km from Delhi) visited a paediatrician in Patna (state capital of Bihar, approx. 300 km from Jharkhand) three times before being referred to a tertiary hospital in Kolkata (state of West Bengal), where he recounts his experience:
The senior doctor said that I cannot treat your child unless you deposit Rs. 8 lakhs right now. I said ma’am I cannot deposit so much money now and the NGO said it would be better if you go to Mumbai. At that time I started thinking how do I go to Mumbai? (…) So I told her that ma’am you are sending us away at 5 o’ clock. You could have told us this same thing the day we came here so that we could have left immediately. Now at 5 in the evening where will I go? So I started crying. I said that how much ever cash I had with me was already spent. So how will I go? (Father of child with ALL)
Another father also described his confused and exhaustive experience of multiple referrals to a paediatrician, orthopaedic surgeon, haematologist and oncologist. Similarly other caregivers acknowledged the delay in timely diagnosis:
The thing is that ma’am, we should have gone to the bigger hospital right at the beginning so that all the checkup is done. We wasted 3-4 days by going to a smaller clinic. So maybe if we would have gone to a bigger hospital then directly it would have been detected (Mother of child with AML)
Efforts taken to visit multiple doctors were often delayed due to geographical issues, especially for those residing far away from diagnostic or treating facilities. Travelling long distances with a sick child was uncomfortable for the family, especially with unreliable public transport systems. Few families had their own transport, but difficult terrain often aggravated the situation.
Determinants influencing the referral pathway
Suggestions were offered by relatives, friends or strangers to seek various medical advice, influencing caregiver health care-seeking behaviours across all hospitals. Most families sought allopathy although few were first influenced to seek treatment through alternate medicine, or visiting the RMP or traditional healer:
Yes the local priest in the village. We got the treatment done through him. Then they had made some medicines and they also did a plan to exorcise jaundice (…) Then in the end I spoke to my family members and showed him to an Ayurvedic doctor in the area. (Father of child with ALL)
Sometimes the opposite advice fast-tracked the trajectory:
Actually, when we went to Srinagar’s [tertiary hospital] we met a patient over there. He told me that if you stay here you will not get cured. Go straightaway to Delhi as they have so many hospitals over there. The treatment will be done immediately. (Uncle of child with ALL)
Mistrust or scepticism of the health system throughout the referral pathway also contributed to delays. This was mainly expressed by the male caregivers, who had a more pivotal role in seeking care. It is presumed their direct involvement and exposure to opinions and experiences shaped their pre-conceived notions of the health system. For example, a few fathers had perceptions of public hospitals being too overcrowded and involving many processes, while others ignored advice to conduct tests in a private hospital.
The issue with government hospitals is that apart from trouble what else do you get there? They make you run here and there. (Father of child with Retinoblastoma)
So we had ignored, because basically in India sometimes private doctors suggest tests for milking money and all. Everybody knows about it. (Father of child with ALL)
Poor knowledge of disease and diagnosis/treatment also acted as a barrier to accessing timely care. Despite visiting multiple health care providers along the referral pathway, some caregivers did not recognise the urgency of the situation to pursue immediate care due to paucity of knowledge. Some families were unaware of cancer and those particularly from rural backgrounds or low SES often questioned the disease aetiology:
I wanted to ask the doctor that since we lie next to him will we also get the same disease? Because the mosquitoes which are biting him are biting us as well. So we should not get the same illness. So this question was coming up in my mind that how can we prevent this illness? Can we also get this infection? (Adult cousin of child with AML)
Many families were unaware of certain tests, radiation or chemotherapy and few thought of researching the disease and procedures while others were afraid to enquire further. Knowledge impacted caregiver confidence but also showed their naivety, some undermining the seriousness of a cancer diagnosis. Some families were therefore prepared to start treatment immediately but others did not understand the urgency of timely diagnosis and treatment. For some caregivers, knowledge increased upon consulting the treating doctor but was also influenced by other families:
So only after we came here, we came to know that this is not a very serious illness. If we are careful about the food and hygiene then my brother will become fine again. So that is why I came to [tertiary hospital] because I had heard that people do get cured over here and go back. (Adult sister of child with PNET)
Patient navigation at the treating hospital
Many families experienced problems in navigating the treating hospital across both cities, especially those who were uneducated. This problem was more prevalent in public hospitals as compared to private hospitals. Time intensive bureaucratic tasks were stressful and discouraging for caregivers rushing to commence treatment. Time was wasted in locating rooms, long queues, completing administrative procedures such as filling forms, applying for reimbursements and registering for diagnostic tests. One teenage boy suffering from PNET took on the labourious administrative tasks himself, including waiting in long queues as described by his mother:
We have to wait for 4 to 5 hours at times. My son wakes up at 3am and gets the [registration] number. Then he tells me that mother you eat and come, I will go ahead. (Mother of child with PNET)
Another mother described her experience in a public hospital before getting her daughter’s bone marrow biopsy done in a private hospital:
Ma’am if we would take our child over there again, then they would have killed her. Because they give such dates that the person will die before that. (Mother of child with ALL)
From the narratives, time estimation between symptom onset and starting the treatment ranged from three weeks to a year, with most families reporting a duration of more than 6 months. Few families had limited visits and were diagnosed at tertiary hospitals near their native home place. Some families from middle-upper SES had more connections with specialists and better knowledge of the referral pathways and treating hospitals than lower SES families, and this advanced their progression toward diagnosis and treatment. Referral pathways for children being treated in Delhi hospitals were more diverse than those treated in Hyderabad. Most families from districts in and around Andhra Pradesh and Telangana had Hyderabad tertiary hospitals as the second or third visit, where they often got a definitive diagnosis and treatment. Families from north Indian states however, had more tertiary hospitals to choose from, either in a neighbouring state or close metropolitan city making their journey longer, although most did not have appropriate diagnosis and treating facilities for children with cancer.
Importance of social supportive care
Although medical care was received intermittently throughout the referral pathway and mainly upon reaching the participating treating hospital, families across both cities often spoke about the need for social support while accessing medical care. Families relied on religious and cultural beliefs (2.1) and it was important to understand the family and social dynamics (2.2) in supporting the primary caregiver financially, emotionally and its subsequent effect on the child. Secondly, upon starting treatment, the ability to stay while receiving treatment (2.3) and health care provider-patient support (2.4) also affected access to medical care.
Religious and cultural beliefs
Religious and sociocultural beliefs influenced the type of support families sought throughout the journey. Alternate treatment was sometimes sought upon symptom onset, and re-visited in conjunction to allopathic care. Although this was more prevalent amongst families from rural or low SES, middle-upper class families also sought alternative care such as one businessman who was treating his son in a private hospital:
We took him to Haridwar to a Vaid
Footnote 1
and his medicines are being given to him. Then we are also giving him the paneer
Footnote 2
made from the milk of the best cow called Gir Gai. And we are also feeding him the pure urine of that cow’s calf as well. (Father of child with Medulloblastoma)
All families expressed a degree of relief using religious means and attributed cause of disease to either an ‘evil eye’, fate or God. Religious influence was also predominant in affecting financial support, showing the extent to which religion played a big role in accessing care:
Among Muslims we don’t even believe in getting insurance done. It is supposed to be illegal. All of that is unnecessary. (Father of child with ALL)
Family and social dynamics
The impact of social and relational roles was evident in the type of support received throughout the journey in both cities. Parents often had to manage other responsibilities apart from taking time out to care for the sick child. Firstly, the opinions of male caregivers regarding the health system (section 1.2) demonstrated that husbands were usually the ones to take the child for health care visits, make decisions and navigate the health system while the female caregivers engaged more in domestic house work. While the shared responsibility might have accelerated the journey, the process was still hindered over time with increasing duties and concerns over the treatment.
Secondly, some caregivers were unable to pursue care due to resource constraints, which were often deliberately withheld by relatives due to domestic conflicts and different set of ideologies. Due to lack of money, one caregiver along with her husband felt it was easier to let her child die naturally believing they could produce more children later who would be healthy:
They thought of not getting the treatment done since it was their first child. They thought of ignoring it is what I felt. They would have ignored and taken her back and left her to her fate. (Uncle of child with Wilms tumour)
Upon reaching the treating hospital, caregivers expressed momentary relief regarding the diagnosis and starting treatment and their confidence grew upon seeing other children also receiving similar treatment. However, some were also apprehensive about the hospital environment. With little to no social support, caregivers from other cities expressed confusion, worry and felt uneasy staying in a new city with unknown people, especially those who were uneducated and from rural backgrounds. Some caregivers spoke of situations of receiving no social support from relatives or friends and leaving behind dependent family members:
The biggest problem is that I have two children whom I have left and come here. My brother is no more. She is my brother’s daughter. I have left everyone and come here since 15 days now. (Uncle of child with Retinoblastoma)
Others expressed gratitude and the significance of a helping family member or non-medical staff of the hospital.
Ability to stay while receiving treatment
A crucial barrier to being able to stay for diagnosis and treatment upon reaching the cancer hospital is finding accommodation. Some caregivers from other cities, particularly those caregivers from a lower SES, were forced to sleep on footpaths, next to metro stations or in government run homeless shelters. This was similar across both cities. The ongoing tests and appointments meant they had to find accommodation close by, and often the child’s health would deteriorate to the point of requiring emergency care. Due to this, even though some families were offered accommodation on the outskirts of the city, they refused it.
I spend the day here and I stay on the road at night (…) I am lying here till evening and I don’t even get food to eat. I don’t get a chance to bathe for 2-3 days at a stretch. (Father of child with Rhabdomyosarcoma)
Once treatment began, caregivers are recommended to provide home cooked food to the patient, which proved challenging for those without appropriate accommodation or facilities. Families including the sick child then resort to eating local unhygienic street food, worsening the condition:
We couldn’t even change our clothes here properly. We would wear the same two sets of clothes regularly for 5 days (…) Today in the morning we had rice and the rice was such that when we made balls out of it and threw it then it started bouncing like plastic. So I don’t know if the rice was made of plastic or not. So that is why we are managing with whatever we are getting. We had thought that if we get a place to stay then we [could store] flour and water and everything. (Adult cousin of child with AML)
Health care provider-patient support
Some caregivers recounted negative experiences from certain health care providers during the referral pathway, where the doctor’s dismissive attitude and inconsistent referrals made them feel insignificant and helpless to progress through the journey:
They gave us too much trouble. She was in a lot of pain. When I would take her to emergency they would say why have you got her here. Take her there! (…) They said they cannot do anything more for her so take her away. (…) [Then] we showed in [out-patient department] but they said go back and show her in emergency. This is how they behaved with us. (Mother of child with ALL)
Upon reaching the treating hospital, the doctor-caregiver relationship was again a recurring matter, where some caregivers expressed confusion, lack of trust and disappointment in health care providers in selected hospitals, while others were satisfied. Upon paying for treatment, a few caregivers appreciated the government or private health insurance schemes available to them, while others were dissatisfied with the application process or financial coverage received. Non-governmental organisations (NGOs) and social worker teams in all hospitals played an important role in supporting those families who were aware of these services. However, unfortunately not all caregivers were aware of the existence of these NGOs.
Accumulative impacts of the journey
There was a clear connection between pathways taken and its accumulated impacts upon families in both cities. Financial impact (3.1) was a common problem for all families which affected the time taken, social relations and quality of care. Ongoing emotional and psychological impacts of the pathway (3.2) refers to the experiences of the caregiver and child resulting in a variety of emotions which facilitated or depleted the will to persevere.
Financial impacts
Financial problems were common for families across both cities. Few families from a middle-upper SES had full or part insurance for their child. Most families who live below the poverty line obtained free or subsidized treatment from state or national government schemes, however some families first had to pay upfront. To pay all expenses most caregivers reported selling off livestock or personal properties and borrowing money or taking a loan. In addition, all caregivers who were the primary breadwinners of the family, had to take leave from work resulting in a loss of income:
He sells vegetables on the cart. The work mainly happens in the evening and the radiation also takes place mainly in the evening. So that becomes a problem because we have to leave the work and come here (Adult cousin of child with Brainstem Glioma)
Caregivers who were dependent on their spouse’s income faced an additional challenge of leaving behind other children to bring the sick child for treatment. Financial impacts were also felt due to external influences, such as the Indian government’s 2017 demonetization policy, where certain Rupee notes became invalid to use, resulting in families unable to spend money to access care. Many caregivers from middle-upper SES acknowledged and empathised with families of lower SES who had financial problems.
Ongoing emotional and psychological impacts of the pathway
Some families recalled sensitive incidents during the referral pathway that burdened them psychologically, especially due to the relationship dynamics between health care providers and families. One father described the situation of being referred back and forth between two hospitals with his daughter who was suffering from extreme body pain:
After going there I felt my condition was like a dog. The child was in so much difficulty and was just wrapped in a towel the entire night crying. (Father of child with ALL)
Impacts were also felt beyond the patient’s family, where additional support was sometimes offered from the community. However, negative psychological and emotional impacts were common across all caregivers interviewed in both cities. Worry, especially over the disease diagnosis, was expressed by all caregivers who understood the diagnosis of cancer:
So I showed the doctor the report and they told me this was the case. I got really scared and started feeling dizzy and I fell. (Mother of child with Non-Hodgkin Lymphoma)
In addition, negative influences from either family or community also placed an added burden upon caregivers:
Others say that this cannot be cured. Why do they say so? They should give the confidence that it can be cured. What has the child done? It’s not fair for such small innocent children to bear this pain. Sometimes I feel instead of seeing this, the child should not have arrived into the world. (Mother of child with Ewing’s Sarcoma)
Caregivers also expressed concern for their own health in many interviews as well as the emotional and psychological impacts upon the child, where older patients who could comprehend the situation expressed their anguish more apparently:
I said Sir please check her (…) I am not lying. She is in a lot of pain. So he said that I cannot admit her and just referred her to a neurologist saying that the child has some problem with her brain (…) The child started crying, she started saying that mother even though I am not crazy they will definitely make me mad now. So I said forget it child, don’t worry. We will consult someone else. (Mother of child with ALL)
link




:max_bytes(150000):strip_icc()/asian-sick-little-girl-lying-in-bed-with-a-high-fever-952683074-5b5b784046e0fb005027ca13.jpg)

